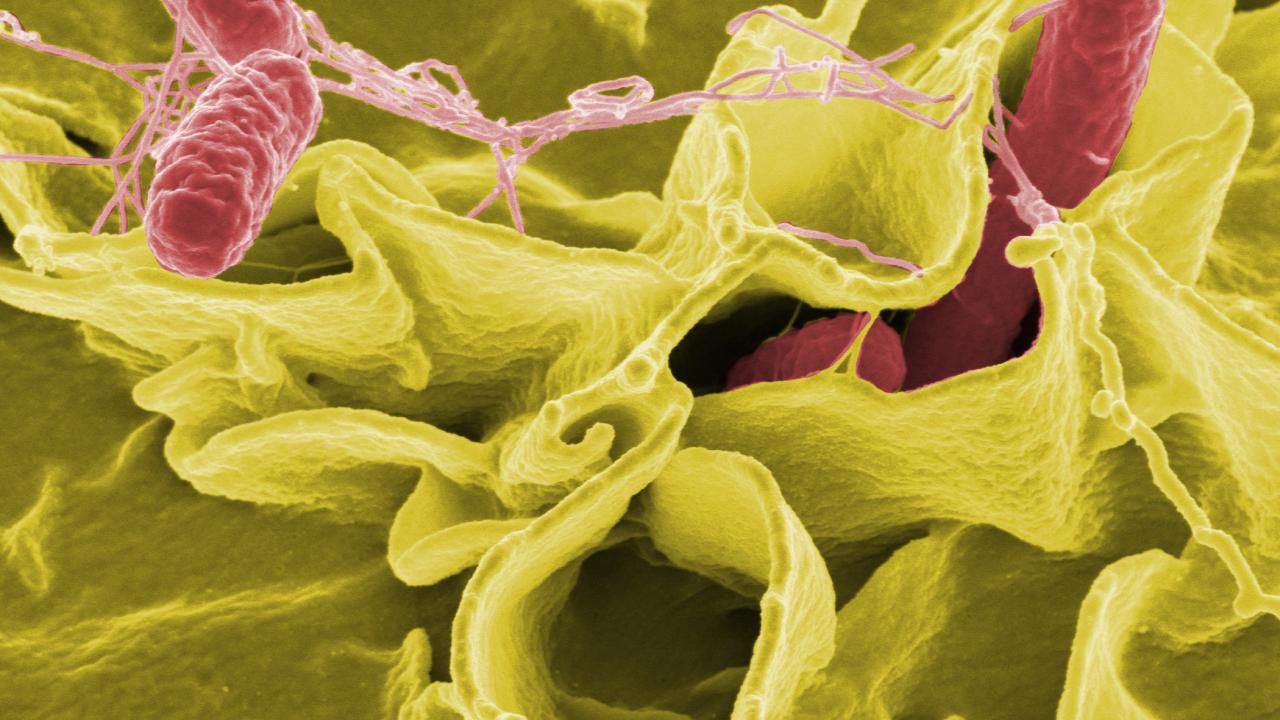
Salmonella infections cause about a million deaths a year worldwide, and there is an urgent need for better vaccines for both typhoid fever and non-typhoidal Salmonella disease. New work from researchers at the UC Davis School of Veterinary Medicine shows how memory T cells, crucial for a vaccine that induces a powerful immune response, can be recruited into the liver in a mouse model of Salmonella.
The work was published April 11 in Proceedings of the National Academy of Sciences.
“Understanding the immunology is key to developing a better vaccine,” said Professor Stephen McSorley, Department of Anatomy, Physiology and Cell Biology and senior author on the paper.
McSorley’s laboratory studies Salmonella, and other bacterial infections such as Chlamydia, in laboratory mice. It’s recently become clear that a type of immune cell called tissue resident memory cells are key to immunity to Salmonella in mice, he said.
When a pathogen enters the body, the immune system mounts a response, including CD4 T-cells which support other responses, such as antibody production by B-cells. When the infection is over, some of the cells specific to that pathogen remain as memory cells, waiting to be called rapidly into service again if the same threat returns.
In the mouse model of Salmonella infection, those CD4 memory T-cells don’t circulate around the body. They hunker down in the liver as tissue resident memory cells.
“We want to know, how do these cells get generated?” said Claire Depew, graduate student in McSorley’s laboratory and first author on the paper. The researchers knew that another type of tissue resident memory cell, CD8 cells, require a signal from the tissue to take up residence. Was the same true for the CD4?
T-cell transfer
To study the problem, Depew adapted an approach used by Australian researchers to study malaria, another disease involving tissue resident memory cells in the liver. She took CD4 T-cells specific for Salmonella and transferred them into mice that had never been infected with Salmonella, so the researchers could study which factors would cause those T-cells to become resident memory cells in the liver.
They found that molecules that promote inflammation, especially interleukin-1 and 2, enhanced formation of Salmonella-specific CD4 tissue resident memory cells in the mice. This provides a rapid-response force that can act quickly against Salmonella infection.
“They’re trained and ready to go,” McSorley said.
The basic science results will help researchers in designing new vaccines for Salmonella, McSorley said.
“A successful vaccine would need to promote conditions to form these cells, without causing liver inflammation,” he said.
Postdoctoral researcher Jordan Rixon was a coauthor on the paper. The work was supported by funding from the National Institutes of Health.