Quick Summary
- Growing cartilage-forming cells under tension improves strength
- Lab-grown material similar mechanical, chemical properties to natural cartilage
- Artificial cartilage could help people with damaged joints, osteoarthritis regain mobility
Biomedical engineers at the University of California, Davis, have created a lab-grown tissue similar to natural cartilage by giving it a bit of a stretch. The tissue, grown under tension but without a supporting scaffold, shows similar mechanical and biochemical properties to natural cartilage. The results are published June 12 in the journal Nature Materials.
Articular cartilage provides a smooth surface for our joints to move, but it can be damaged by trauma, disease or overuse. Once damaged, it does not regrow and is difficult to replace. Artificial cartilage that could be implanted into damaged joints would have great potential to help people regain mobility.
Natural cartilage is formed by cells called chondrocytes that stick together and produce a matrix of proteins and other molecules that solidifies into cartilage. Bioengineers have tried to create cartilage, and other materials, in the lab by growing cells on artificial scaffolds. More recently, they have turned to “scaffold-free” systems that better represent natural conditions.
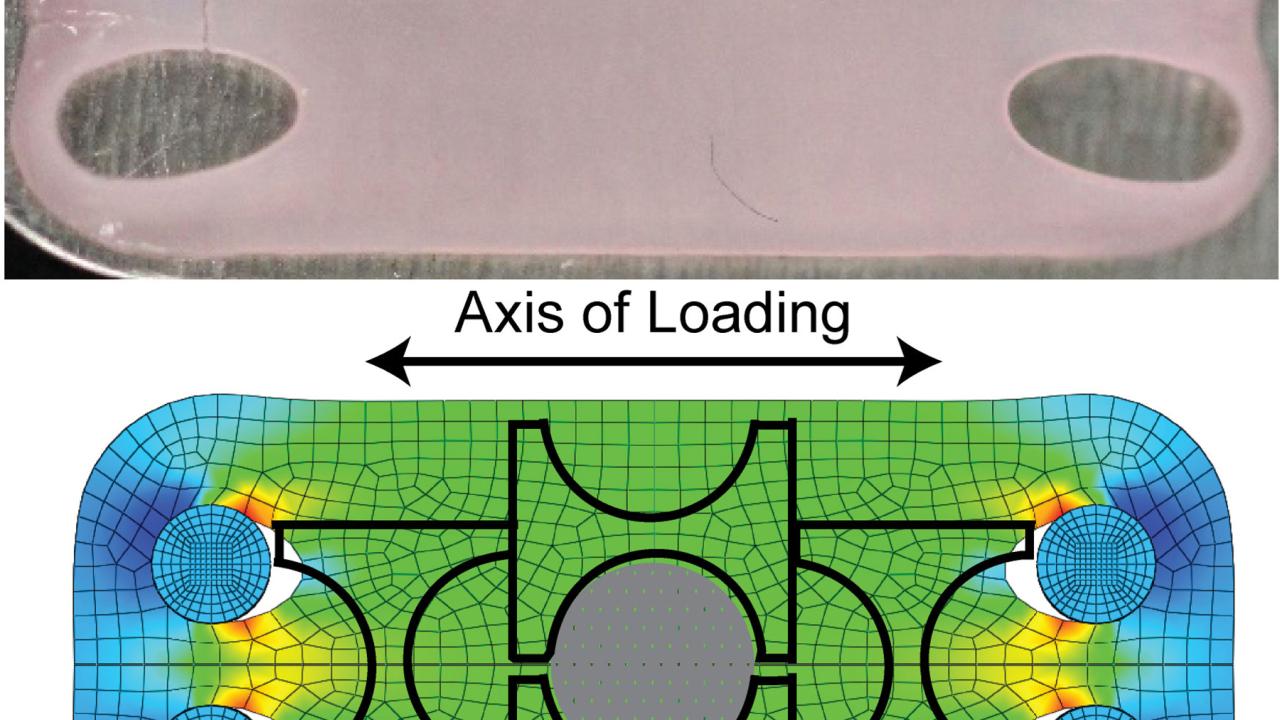
The UC Davis team, led by Professor Kyriacos Athanasiou, Department of Biomedical Engineering, grew human chondrocytes in a scaffold-free system, allowing the cells to self-assemble and stick together inside a specially designed device. Once the cells had assembled, they were put under tension — mildly stretched — over several days. They showed similar results using bovine cells as well.
“As they were stretched, they became stiffer,” said Jerry Hu, a research engineer and co-author on the study. “We think of cartilage as being strong in compression, but putting it under tension has dramatic effects.”
The new material had a similar composition and mechanical properties to natural cartilage, they found. It contains a mix of glycoproteins and collagen, with crosslinks between collagen strands giving strength to the material.
Experiments with mice show that the lab-grown material can survive in a physiological environment. The next step, Hu said, is to put the lab-grown cartilage into a load-bearing joint, to see if it remains durable under stress.
“In this comprehensive study, we showed that we can finally engineer tissue that has the tensile and compressive characteristics of native tissue,” Athanasiou said. “The artificial cartilage that we engineer is fully biological with a structure akin to real cartilage. Most importantly, we believe that we have solved the complex problem of making tissues in the laboratory that are strong and stiff enough to take the extremely high loads encountered in joints such as the knee and hip.”
Additional authors on the paper are: co-first authors Jennifer Lee and Le Huwe, Nikolaos Paschos and Ashkan Aryaei, all at UC Davis; and Courtney Gegg, now a graduate student at Stanford University. Athanasiou also holds an appointment as professor in the UC Davis Department of Orthopedic Surgery. The work was supported by grants from the National Institutes of Health.
Media Resources
Andy Fell, News and Media Relations, 530-752-4533, ahfell@ucdavis.edu
Kyriacos Athanasiou, Biomedical Engineering, (530) 752-1033, athanasiou@ucdavis.edu